Have you heard about the Gut Brain Connection? They say that the gut is the second brain. However, you can argue that the gut is at least the co-brain, if not the brains of the whole operation! Our gut is home to thousands upon thousands of tiny microbes that work around the clock to keep us ticking. So when the good bugs in our belly get outnumbered by pathogens, it negatively affects our day-to-day life. From stress to hormone production to mood swings, brain fog and more.
I’ve experienced this first hand. Brain fog so bad I couldn’t work or function to carry out the most simple tasks. Not being able to cope with situations that would have been easy to manage at other times. Let’s dive deeper on the gut-brain axis and what you can do to strengthen the connection.
Is the Gut-Brain Axis a Real Thing?
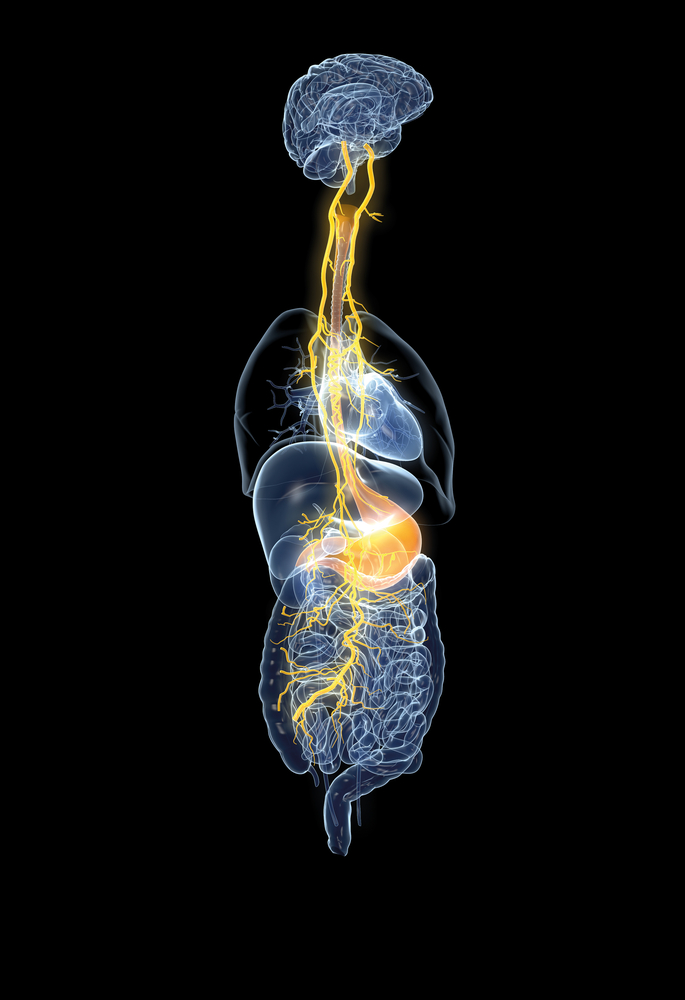
There is a genuine connection between the gut and the brain. The gut-brain axis is actually a biological pathway that links the central nervous system (CNS) and the enteric nervous system (ENS). Along the main road between the gut-brain axis boasts several direct and indirect pathways to other areas of the body. Therefore, it has the ability to communicate with:- Autonomic Nervous System (ANS) – This is the part of the body that takes care of the things that we don’t think about such as breathing and cell reproduction. It is broken into three distinct parts:
- Endocrine System (Hypothalamic-Pituitary-Adrenal Axis or HPA axis) – This is a group of organs that are responsible for many important functions such as hormone production, mood, and regulating the sleep cycle.
- Parasympathetic System – In charge of resting and digestion. It’s main purpose is to conserve energy and does so by doing things such as slowing down the heart rate and relaxing sphincter muscles.
- Sympathetic System – Our fight-or-flight response to situations. This system plays a role in creating hormones such as adrenaline or cortisol.
- Immune System – Cells, tissues, and organs work together to keep the body free of foreign cultures.
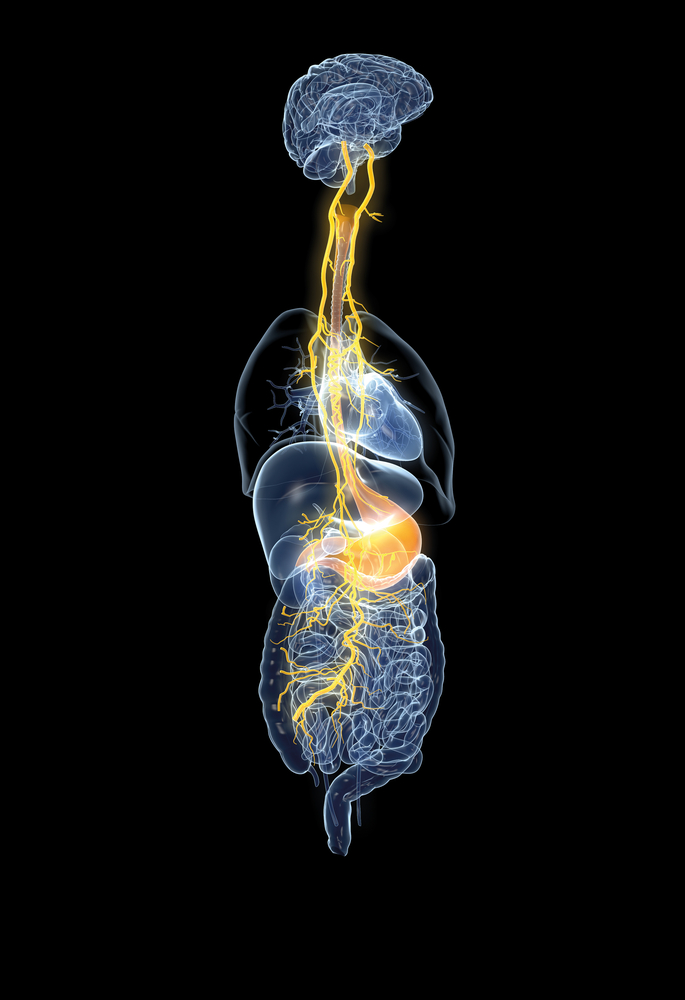
Gut to Brain – A Direct Line of Communication
One has to wonder…did the gut form the brain? This might sound far-fetched at first, but think about it. A fetus is formed in the mother’s womb. Its first exposure to life is their mother’s vaginal microbiota. The interaction between this new form of life and those bacteria shapes the immediate growth and future development of this human being’s CNS and ENS. So the exact bacteria that saw a child born from egg to human played a huge role in the creation of everything we see on our body head to toes. It also formed what we think and how we feel. From birth, our gut has had open communication with our brain. It achieves this through many modes. These include:- Vagus Nerve – Sensory neurons travel down this most direct link between the brain and gut. The intestines signal to the brain stem what’s going on in the gut, which engages the limbic system. This is where your emotions lie. When your intestines are unhappy, you will feel stressed, triggering cortisol production and in turn, negatively impacts the gut. This creates a downward cycle of poor gut and mental health.
- Leaky Gut Syndrome – When we are under chronic stress, it begins to change our microbiome. As more cortisol pumps into the body, it can clog up your gut. In turn, your environment can become more acidic, causing it to break the gut barrier. The end result is Leaky Gut Syndrome. This condition has been scientifically linked to mental health disorders such as depression due to the amount of toxins in the bloodstream.
- Gut Hormone Signalling – Many bacteria present in your microbiota may stimulate enteroendocrine cells. When excited, these cells produce neuropeptides, such as glucagon-like peptide 1 and substance P (pain). As neuropeptides enter the bloodstream, they can directly affect the ENS. When this happens, you may feel stomach conditions such as Inflammatory Bowel Syndrome (IBS).
- Tryptophan Metabolism – In order to create serotonin, the happy neurotransmitter, you need the amino acid, tryptophan. When the body’s gut mucosal enterochromaffin cells digest tryptophan, it creates ~90% of the serotonin in your bloodstream. So, literally if your gut is unhappy…you will be unhappy!
- Good Bacteria Putting in Work – The gut doesn’t need to be a scary place. Many helpful bacteria live there. After all, that’s how you came into existence. These things know what they’re doing. For instance, bacteria species such as Bifidobacterium and Lactobacillus create gamma-aminobutyric acid (GABA), which is a neurotransmitter that tells the brain to feel calm. Many others produce amino acids and other proteins we need (and take for granted).
Gut Health and Mental Health
When you are under an immense amount of stress, do you sometimes feel sick to your stomach? Now think of your first love. Back in the day, did you used get those feelings of butterflies? These are living embodiments that the gut-health connection is real on two opposite ends of the spectrum. Let’s take a look at these two feelings.Negative Impact of Gut Health on Mental Health
If you are ever in what you perceive as a stressful situation, the amygdala in the brain tries to process your emotional response. By interpreting the information present in this stressful situation, the brain sends stress signals in the form of neurons to the hypothalamus. The hypothalamus starts up the sympathetic system and sends autonomic nerve fibers over to the adrenal glands in the HPA axis. This is where we create the hormone, cortisol. Our body can only hold so many hormones. So, if we produce cortisol every time we feel stress and stress becomes chronic, which hormone do you think we will produce the most of? Not melatonin, the sleep hormone. Not estrogen or testosterone. Nope. Cortisol! Studies have shown that excess cortisol converts to fat. As fat begins to pile up, this is really the precursor to many fatal illness such as cardiovascular disease, diabetes, and cancer. Therefore, chronic stress is a breeding ground for disease. This isn’t where the negative gut-brain ties end. It only gets more complicated from there. Bad bacteria in the gut has been linked to many mental health and other conditions such as:- Autism – Studies suggest that bacteria transmitted in utero may play a big role in autism. In fact, one found that high levels of the bacteria Clostridium and Desulfovibrio alters brain development behavior to exhibit symptoms of autism.
- Schizophrenia – Studies show that patients diagnosed with schizophrenia tend to have increased levels of Lactobacillus casei, Lactobacillus lactis, Streptococcus mutans and Streptococcus thermophilus. These all alter the Th2 immune response seen in cases of schizophrenia.
- Depression – Speaking of Clostridium, this pathogenic bacteria produces HPHPA and p-cresol, these are acids and microbial metabolites respectively. More importantly, they stop the growth of the enzyme, dopamine beta-hydroxylase. As the name suggests, this is responsible for the production of our happy hormone, dopamine.
Positive Impact of Gut Health on Mental Health
On the flip side of things, the gut can also do a lot of good for the body. Remember those feelings of butterflies? That’s the gut-brain connection at work. There’s a lot going on when this happens. For one, your HPA axis is doing it’s thing again. This time for the greater good, the adrenal glands are pumping out the hormone adrenaline. As a heads up, it might be secreting some cortisol too. That’s the feeling that maybe you should run and hide when you like someone. However, when the adrenaline kicks in, you begin to feel those fireworks. In turn, it causes the ANS to contract your stomach muscles, making that butterfly effect.How to Improve the Gut-Brain Connection
So how do we live by the mantra, “Happy gut, happy brain?” Here are a few easy ways to help improve the gut-brain connection.-
- Probiotics Supplements and fermented foods – As you’ve put together by now, there’s a lot of good bacteria out there. Sometimes our body needs more of them. As the bad bacteria wins over in your gut, you need more live probiotics to help fight them off. For really severe conditions, you can even get your microbiome tested. From there, companies can formulate personalized probiotics supplements based on the good bacteria you have lacking and the bad bacteria you have winning.
- Diet – Think long and hard about what you’re eating and how your body is responding. Look in to some gut healing foods and switching to a wholefoods diet and be sure ditch any processed foods. Keep a food journal and write down how you feel and see if you notice any patterns. Listen to your body. It’s trying to tell you something!
- Exercise – Exercise can help create endorphins. This helps us feel happy. Therefore, with time you will actually see exercise as an exciting thing to do. Not to mention, you’ll love losing the extra kilos…and so will your gut. Exercise also gets your lymphatic system pumping, helping remove toxins from your body. Recent studies have revealed that HIIT (High Intensive Interval Training) can have a positive effect on your microbiome.